LISTEN TO THIS ARTICLE:
Collective trauma
We are facing the greatest threat to our collective and individual health that the world has experienced in generations. New York City, America’s largest city, is now the worldwide epicenter of the COVID-19 outbreak, and our other urban areas may not be far behind. Nine out of ten Americans are now under some type of stay-at-home order, or live in an area that has at least closed non-essential businesses. By now, even the most rural areas of our country have been touched by the outbreak. From a mental health perspective, what we are experiencing can be termed a collective COVID trauma.
Every one of us has been or will be touched in some way by this. Invisible and deadly, none of us can know where and when it will strike next. We are waking each day to a bigger dose of fear than the day before. And while most of us are aware of the terrible physical toll of this disease, what about its impact on our mental health? We should pay close attention because maintaining a healthy mind now is crucial to recovery. So what are the mental health effects and how do you head them off during this pandemic?
While most of us are aware of the terrible physical toll of this disease, what about its impact on our mental health? We should pay close attention because maintaining a healthy mind now is crucial to recovery.
Why this is different from other disasters?
For the past month, every day has felt worse than the previous one. We keep hearing about the numbers of people sick, hospitalized, or dying. These numbers seemed unthinkable just a few weeks ago, when this invisible threat was still foreign, and removed from our everyday lives. For most of us, the threat of death is a long way off. Perhaps for older adults, those with serious health problems, or people with dangerous jobs, it may seem more pressing. In general, though, our mortality is not often at the forefront of our minds. It is now.
For most of us, the threat of death is a long way off. In general our mortality is not often at the forefront of our minds. It is now.
We have lived through group trauma before. The 9/11 terrorist attacks are the most recent comparable event. Anyone old enough to have experienced that day and the weeks that followed, can remember the stunning images played over and over on television. Natural disasters come to mind, as well. Rampaging fires and ferocious hurricanes destroy homes and displace thousands every year. Even mass shootings, which are more physically localized events, hit hard for everyone.
This will change our lives
But this is different. Our country is vast, and most of these disasters are at least somewhat geographically isolated from large swaths of America. The past few months have proven that coronavirus does not respect any type of boundaries. Past traumas were shorter as well. Hurricanes last a few days, terrorist attacks and mass shootings are single-day events. Only major fires come close to the timeline that the coronavirus is taking.
There’s a good chance those who aren’t [infected] will have a friend or family member who is. This is the very essence of trauma.
Perhaps the most frightening part of the virus is how stealthily the threat moves. The virus has silently swept around the world before we knew what hit us. It has shattered our sense of security and brought the risk of death closer to home for all of us. Millions will likely be infected, and there’s a good chance those who aren’t will have a friend or family member who is. This is the very essence of trauma.
The risks of developing a stress-related disorder
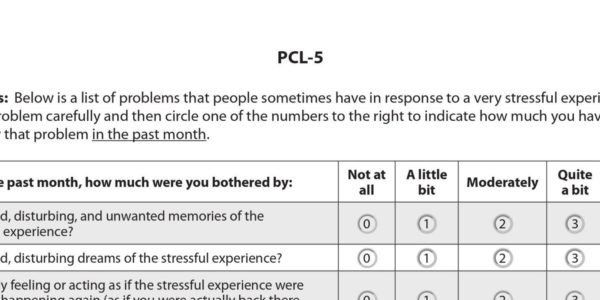
The shock of COVID to our individual and collective mental health is incredibly stressful. It’s the type of situation that can potentially lead to stress disorders like Post Traumatic Stress Disorder (PTSD) and Acute Stress Disorder. Stress disorders appear after people have suffered (or witnessed others suffer) a serious threat to their life or health. People with these disorders have flashbacks and nightmares about the trauma and need to avoid reminders of it. Their stress response systems are turned up, and they always feel on edge.
Most people associate PTSD with survivors of war. For the people working in hospitals during this pandemic, this is a war, and they are on the front line. They see firsthand the terrible toll of the virus.
Those who work in essential industries, like those who keep our nation supplied with food and other necessities, are not directly subject to the horrors of this disease, but they are certainly at high risk. They continue to work, regularly coming into contact with others. The rest of us are stuck at home, and authorities tell us the best thing we can do to help is to do nothing.
Who is most at risk?
Many factors contribute to who develops stress disorders. One of the strongest predictors is the severity of the stress, and healthcare workers will be among those at the highest risk. Anyone who gets sick with coronavirus (especially if hospitalized), or whose loved one becomes ill or is hospitalized, is at risk of developing a stress disorder. People who are sheltering in their homes and who never face the virus firsthand are slightly less likely to develop a stress disorder, but all of us are still suffering a crisis en masse.
Hundreds of millions of people are confined, mostly to their homes. About ten million have lost their jobs so far. Those who are alone face isolation, while homes of families or roommates can become crucibles for human conflict. We are already seeing a wave of reports of domestic violence in places under quarantine and stay-at-home rules.
What happens to people with existing mental health conditions?
People with existing mental health or substance use disorders are facing mental health troubles as well due to COVID. Those who rely on regularly meeting in groups to support each other can’t meet and are at risk of relapse. The constant stream of news from the outbreak hot spots is difficult for anyone to bear, let alone those already dealing with depression or anxiety. For individuals with Obsessive-Compulsive Disorder, germ phobia, or Illness Anxiety Disorder, all of whom experience severe anxiety about getting sick, it can be overwhelming. The coronavirus is also likely to feed delusions or paranoia, as in people with Schizophrenia. People in these groups will need additional support during the coming months, adding to the demand already straining our healthcare system.
How to head off the effects of trauma
While we are playing catch up in managing the surge of coronavirus cases, we may be able to head off some of the more intense emotional effects of the trauma, both as individuals and as a society. We are in a unique situation where we can reflect on the trauma as we are experiencing it.
Practice acceptance
As is typical in traumatic situations, a profound sense of helplessness can overwhelm us and we must try to manage those feelings. One of the simplest and best techniques we can use right now is the concept of acceptance. This means accepting that we cannot control the vast majority of the terrible things that happen in the world. Acknowledging our powerlessness is a critical step in substance use recovery and anxiety management, and right now, it offers a fundamental approach to dealing with the helplessness we are all feeling.
Give yourself a news limit
We cannot change the past, and we have very little control over the future. There are greater forces at play in the world than what any one of us can command. This pandemic will eventually be over, and the time we spend watching TV, reading the news, and mulling over the gruesome facts will not change the how or the when. Give yourself a news limit for each day, where you check a few sources for a limited period of time, then be done with it.
Use mindfulness
Mindfulness provides another concept related to acceptance that is vital for us. When you find yourself obsessively worrying about the next day, week, or month, take a moment to bring yourself back to the present. Even if you only have a few minutes, this will help. Find a place to sit; the quieter, the better. Place one hand on your chest and the other on your belly. Breathe in through your nose for 4 seconds, hold it in 4 seconds, breathe out through your mouth for 4 seconds, and finally hold your breath out for 4 seconds. Focus on the sensation of air passing in and out of your mouth and nose throughout this time. This technique, known as “square breathing,” is a simple form of meditation. It tones down the body’s stress response systems, slows racing thoughts, and tames the symptoms of anxiety.
Find a safe way to offer help
Once we have taken time to address our own needs, we can go out and try to help others. Around the country, people are reaching out to help those in need around them. You can help get groceries for people who can’t leave their homes, volunteer to (virtually) visit those in nursing homes, donate blood, or even sew masks if you can. When we help others, we are often surprised to find that it gives us strength. Here are two sources to help you get started, organized by group in need and area. They can connect you with ways to offer help and request assistance if you need it.
Find the silver lining
When we take a moment to step back from the chaos engulfing our country and world, we discover that there may be a silver lining to this crisis. But we may have to work to find it. The effort we put into building our mental strength now will pay off in the long term. If we approach this as a challenge to be surmounted, rather than a horror, we can find a sense of purpose and, most importantly, hope.


 Learn
Learn ID Symptom
ID Symptom News
News Find Help
Find Help
 Share
Share
 Share
Share
 Share
Share
 Share
Share